What is Upper Endoscopy (EGD)?
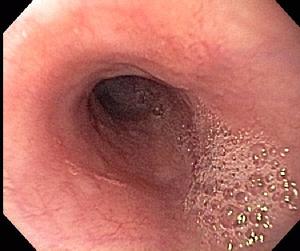
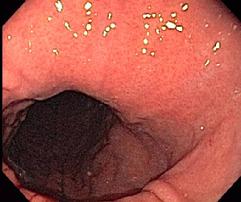
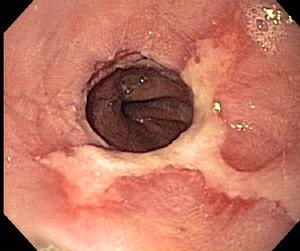
Upper endoscopy, also called EGD (EsophagoGastroDuodenoscopy) or gastroscopy, is an examination of the esophagus, stomach and duodenum (first section of the small intestine) performed by having you swallow an endoscope, usually while sedated.
The endoscope is a long, thin, flexible and steerable tube, about the diameter of a small finger, which passes easily through your mouth and throat structures following the natural food path.
Why is Upper Endoscopy Performed?
Upper endoscopy is performed to evaluate the esophagus, stomach and duodenum for a variety of disease processes which affect the interior lining of these organs, or block the normal passage of food and secretions through the upper intestines.
Common conditions we evaluate and treat include:
- Gastroesophageal reflux disease (GERD)
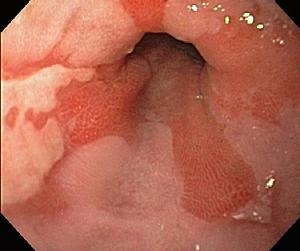
- Eosinophilic esophagitis
- Esophageal infections
- Helicobacter pylori gastritis (stomach infection)
- Ulcers of the esophagus, stomach and duodenum
- Bleeding from the upper intestinal tract
- Barrett's esophagus
- Esophageal strictures
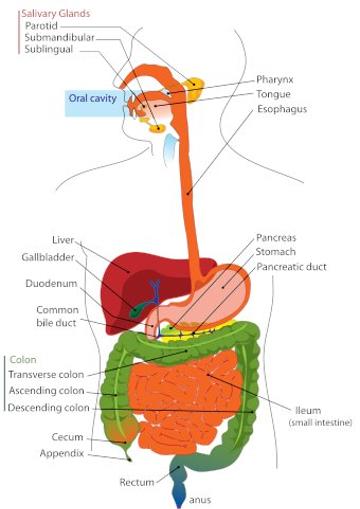
Anatomy of the upper digestive tract